COLUMN: Our health systems are overwhelmed
June 7, 2022
This past weekend, I had to make a trip to the emergency room. When I arrived, I went straight to a triage room so they could access the level of my severity. I was not actively having cardiac arrest or an allergic reaction, so I was low on the priority list. But I was still in pain and using a wheelchair.
My dad and I checked in around 1:45 p.m. and sat in the waiting room until they called my name. We sat there for quite some time. Around 4:15 p.m. we were finally called back. We got to my room and the nurse practitioner realized that I had not done some of the things they needed me to do. It had simply been lost in the commotion.
Around 6 p.m. I was taken to imaging to get a CT scan. This was the fastest process of the entire day. It took about another hour for them to process and read the image. Then about another hour for them to gather my paperwork and finally release me.
While sitting in my room, I watched many nurses and doctors whiz by just trying to make it to the next patient. I could tell these professionals were just trying to make it to the end of their shift. It was a Sunday afternoon/night, and they were exhausted.
Between COVID-19 patients and the everyday emergency patients, our health care systems are in overdrive. They are trying to care for patients with low resources and staff. Every day these professionals are caring for our most vulnerable population and those who are injured, but they are treated so poorly. There are signs everywhere that say “we support our healthcare workers” but they still work long hours for low pay. They are trying to care for patients with minimal supplies and personnel.
How can our health care professionals do their best work when they are so understaffed and low on resources? How can people get the best health care help when professionals are stretched so thin? More than 20 percent of health care professionals quit their job due to the COVID-19 pandemic. They simply stated they were emotionally and physically burnt out, according to a PEW Research Center article.
The United States is short 20,000 doctors to meet the health care needs of the country, according to the Association o American Medical Colleges. If that is not scary enough, the same team estimated that the gap could increase to 124,000 by 2034. The workforce studied director of the team, Michael Dill, stated that within the next 10 years, two of every five physicians in the workforce will be 65 or older.
There is a lot to think about while waiting eight hours in an emergency room. I just did not expect my sciatic nerve damage to take a back seat in my thoughts while trying to analyze the environment around me. More support for healthcare professionals now and in the coming years is necessary. We must support our professionals to keep an effective and functioning health care system. Because without a functioning healthcare system, we are about to wait a little more than eight hours in the emergency room.
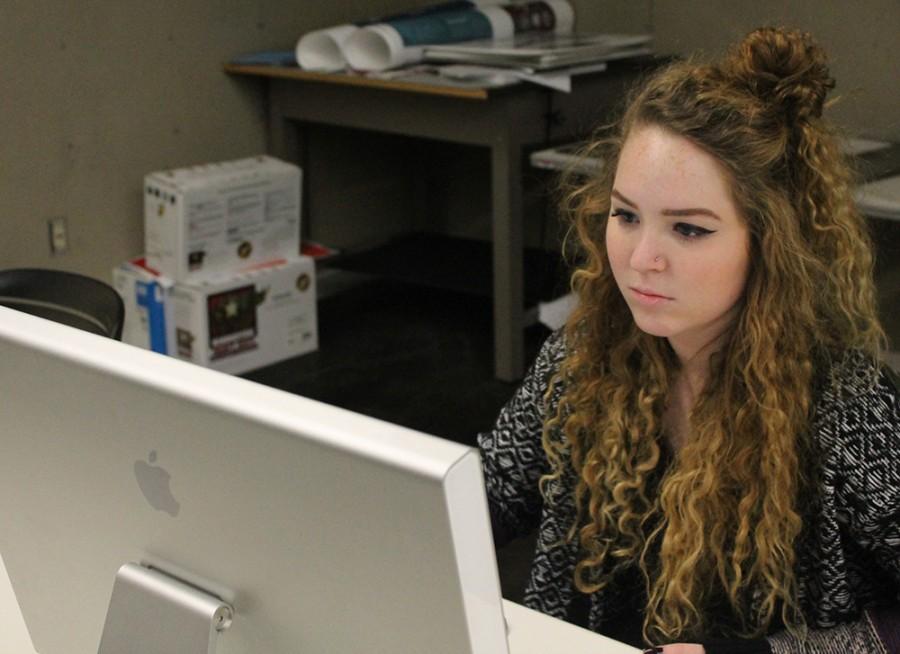
Ellen Dooley is a sophomore special education standard major. She can be reached at 581-2812 or [email protected].